BRAIN LAB COMPUTER NAVIGATION SYSTEM
- Easy and direct access to sensitive areas of brain.
- Pin point definition of eloquent areas of brain like motor, speech and visual centres..
- Maximizes surgical precision..
- Useful in brain tumors, aneurysms, AVMs,and functional neurosurgery..
Z-TOUCH MARKERLESS
- Wireless laser registration pointer with pinpoint accuracy.
- No facemask, headset or markers needed.
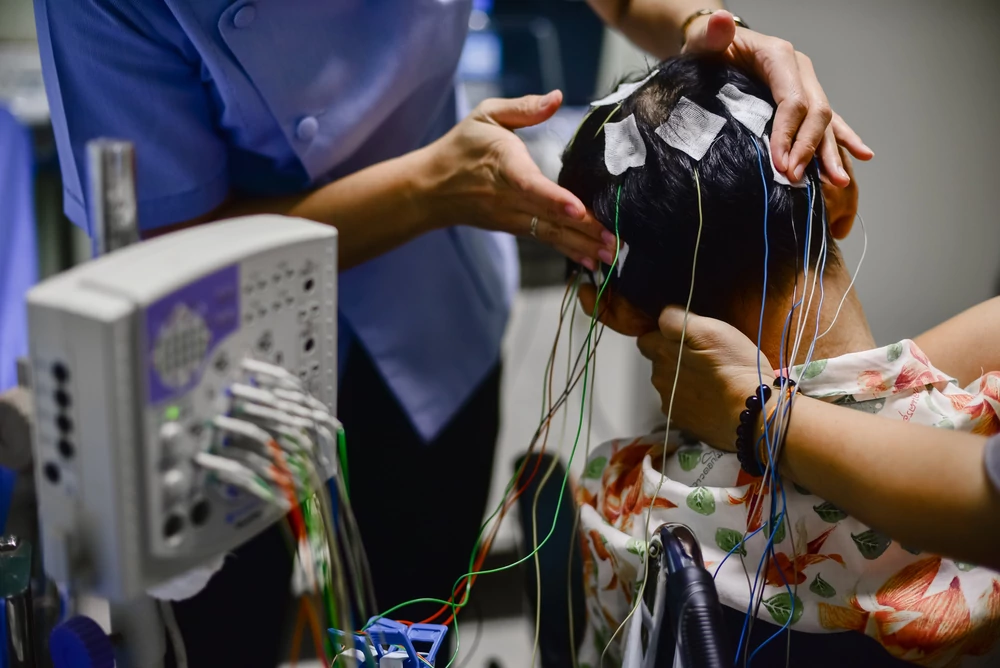
Well-equipped Neuro surgery and Neurology outpatient consultation area with spacious consultation chambers in the Neuro Science and Spine Block.HINS has a modern neuro-diagnostic lab, which has EEG, ENMG and Nerve Condition Study facilities. We have state-of-the-art GE Hi-Speed Spiral CT Scanner, which performs highly specialized CT studies like perfusion studies, high speed CT Angiography, virtual endoscopy etc. HINS has the only open type, non-claustrophobic MRI system in the city, which gives high quality images with minimum patient discomfort. We have 10 well-equipped, modern operation theatres, complimented by a sophisticated ICU equipped with ventilators and monitors.
ELECTROENCEPHALOGRAPHY(EEG)
The electroencephalogram (EEG) is a medical test used to measure electrical activity of the brain, via electrodes applied to your scalp. This procedure is completely painless and can be performed without shaving any of your hair.
- EEG tests are appropriate diagnostic indicators in relation to some of the following diseases: Epilepsy.
- Non-epileptic paroxysmal disorder.
- Neurologic lesions
- Cerebrovascular disorders.
- Brain tumor and other intracranial spatial disorders.
- EEG examination during and after neurosurgery and stereotaxic brain surgery.
EMG stands for Electromyogram which translated means electrical testing of muscles but in fact has come to mean electrical testing of nerves and muscles. EMG is an in-office procedure and does not require hospitalization. On average, an EMG takes anywhere between 30 minutes to 2 hours.
EMG IS DONE FOR DIAGNOSING THE FOLLOWING CONDITION:
- Inflammatory Demyelinating Neuropathy.
- Chronic Inflammatory Demyelinating Polyradiculoneuropathy.
- Myasthenia Gravis.
- Carpal Tunnel Syndrome.
- Parkinson’s disease.
- All neuropathies, Myopathies, Radiculopathies.
With all these supportive systems the Department of Neurosciences is well-poised to offer high-quality neurological care with excellent support from comprehensive Physiotherapy & Occupational therapy departments. A holistic approach to the patient’s concerns and disabilities are well assured.
All members of the department are committed to deliver the best possible care to each and every patient who enters HOSMAT. We bring back smiles on patients face!
HEAD INJURY: ROAD TO RECOVERY
Head injury (HI) is a major public health problem. It occurs most commonly in teenagers and young adults who would otherwise have been productive members of society. The disabilities that many of them incur from their head injuries often make them dependent upon rehabilitation services for the rest of their lives. Although head injuries steal away more potentially productive years than such common illnesses as cancer, AIDS, heart disease, and diabetes, less research money is spent on head injury than on these other diseases. The most common cause of head injury is motor vehicle accidents. Alcohol & drug use contributes significantly to the occurrence of many head injuries.
WHAT GOES WRONG?
When discussing head-injured patients, neurosurgeons often use the term “mass lesion”, which refers to an area of localized injury that may cause pressure within the brain. The most common mass lesions seen after head injury are hematomas and contusions. A hematoma is a blood clot within the brain or on its surface. A contusion may be thought of as an area of “bruised” brain. When examined under a microscope, cerebral contusions are comparable to bruises in other parts of the body. They consist of areas of injured or swollen brain mixed with blood that has leaked out of arteries, veins, or capillaries. Hematomas and contusions can occur anywhere within the brain. Those hematomas between the skull and the dura, which is a thick membrane that surrounds the brain, are called epidural hematomas. Hematomas that are between the dura and the surface of the brain are called subdural hematomas. Intracerebral hematomas are blood clots that are located within the brain tissue itself. Contusions are seen most commonly at the base of the front parts of the brain, but they can occur anywhere. Subarachnoid hemorrhage appears as diffuse blood, spread thinly over the surface of the brain. This is seen commonly after head injury. If this is the only abnormality present on a CT scan, then observation for a short period may be the only treatment needed.
DIFFUSE INJURIES
The hematomas and contusions described above generally occur in only one or a few specific parts of a patient’s brain, and they are usually easily seen on a computerized tomography (CT) scan. However, HI can also produce microscopic changes that cannot be seen on CT scans and that are scattered throughout the brain. This category of injuries is called diffuse brain injury, which can occur with or without an associated mass lesion. One type of diffuse brain injury is diffuse axonal injury. This refers to impaired function and gradual loss of some axons, which are the long extensions of a nerve cell that enable such cells to communicate with each other even if they are located in parts of the brain that are far apart. If enough axons are injured in this way, then the ability of nerve cells to communicate with each other and to integrate their function may be lost or greatly impaired, possibly leaving a patient with severe disabilities. Another type of diffuse injury is ischemia, or insufficient blood supply to certain parts of the brain. It has been shown that a drop in blood supply to very low levels may occur commonly in a significant percentage of head-injured patients. This is important because a brain that has just undergone a traumatic injury is especially sensitive to even slight reductions in blood flow. For the same reason, changes in blood pressure during the first few days after head injury can have an adverse effect.
SKULL FRACTURES
No treatment is required for most linear skull fractures, which are simple breaks or ” cracks” in the skull. Of greater concern is the possibility that forces strong enough to cause a skull fracture may also have caused some damage to the underlying brain. Fractures of the base of the skull are worrisome if they cause injury to nerves, arteries, or other structures. If a fracture extends into the sinuses, there may be leakage of cerebrospinal fluid (CSF) from the nose or ears. Most such leaks will stop spontaneously. Depressed skull fractures are those in which part of the bone presses on or into the brain. These may require surgical treatment. The damage caused by depressed skull fractures depends upon the region of the brain in which they are located and also upon the possible coexistence of any associated diffuse brain injury.
ASSESSMENT
Like all trauma patients, persons with head injury need a systematic yet rapid evaluation in the emergency room. Cardiac and pulmonary function are the first priority. Next, a rapid examination of the entire body is performed.
NEUROLOGICAL EXAMINATION
An accurate neurological examination is important to plan further evaluation and possible treatment. The standard for objectively assessing the severity of head injury is the Glasgow Coma Scale (GCS). This scale assigns points to each patient based upon three categories: verbal function, eye opening, and best motor(movement) response. Patients with a GCS score of 13-15 are usually classified as having mild head injuries. Those with a GCS score of 9-12 have moderate head injuries, and those with a score of 3-8 are usually described as having severe head injuries. In addition to the GCS, the ability of the pupils to become smaller in bright light is also important after head injury. In patients with large mass lesions one or both pupils may be very wide or ” blown”. The presence of a wide, or dilated, pupil on only one side suggests that a large mass lesion may be present on the same side as the dilated pupil.
TREATMENT – SURGICAL
Many patients with moderate or severe head injuries are taken directly from the emergency room to the operating room. In many cases, surgery is performed to remove a large hematoma or contusion that is significantly compressing the brain or raising the pressure within the skull. After surgery, these patients are usually observed and monitored in the intensive care unit (ICU).
MEDICAL
At the present time, there is no drug or “miracle treatment” that can be given to prevent nerve damage or promote nerve healing after HI. The best treatment that can be performed in an ICU is to prevent any secondary injury to the brain. The “primary insult” refers to the initial trauma to the brain, whereas a “secondary insult” is any subsequent development that may contribute to neurologic injury.
REHABILITATION
Once they leave the acute-care hospital, head-injured patients may benefit from an aggressive rehabilitation program. Another major goal of head injury rehabilitation is working with patients’ families to educate them about what they can realistically expect and how they can best help their injured family member.
ROAD TO RECOVERY
Tremendous effort is being directed into finding better ways to evaluate these problems, into improving the quality of pre-hospital, acute, and rehabilitative care, and into research to learn more about the effects of head injury and their possible treatment, keeping these points in mind – HOSMAT Hospital the pioneers in Orthopaedics & Accident Trauma Care in Bangalore, now envisages in providing super specialty treatment in the following specialties – neuro sciences, spinal surgery, arthritis and joint replacement by inaugurating the HOSMAT Super Specialty Hospital. The state of the art super specialty hospital in the country having 75,000sq feet modern building, this new hospital wing in the same campus in addition to the 75,000 sq. ft. of the existing hospital with 250 new beds, making HOSMAT a 500 bed Orthopedic, Neuro Sciences & Accident Trauma Hospital, the largest in the country with 12 Hi Tech OT’s , 25 bed ICU, 20 consultation chambers, equipped with advanced Neuro surgical Microscope, Sophisticated Computer Navigation System (for Neurosurgery, Joint Replacement & Spine Surgery), MRI, CT, EEG , ENMG, a 24-hour Orthopedics, Neuro sciences & Accident Trauma Centre.
HEADACHE MAY BE A ‘PAIN IN YOUR HEAD’!
Tremendous effort is being directed into finding better ways to evaluate these problems, into improving the quality of pre-hospital, acute, and rehabilitative care, and into research to learn more about the effects of head injury and their possible treatment, keeping these points in mind – HOSMAT Hospital the pioneers in Orthopaedics & Accident Trauma Care in Bangalore, now envisages in providing super specialty treatment in the following specialties – neuro sciences, spinal surgery, arthritis and joint replacement by inaugurating the HOSMAT Super Specialty Hospital. The state of the art super specialty hospital in the country having 75,000sq feet modern building, this new hospital wing in the same campus in addition to the 75,000 sq. ft. of the existing hospital with 250 new beds, making HOSMAT a 500 bed Orthopedic, Neuro Sciences & Accident Trauma Hospital, the largest in the country with 12 Hi Tech OT’s , 25 bed ICU, 20 consultation chambers, equipped with advanced Neuro surgical Microscope, Sophisticated Computer Navigation System (for Neurosurgery, Joint Replacement & Spine Surgery), MRI, CT, EEG , ENMG, a 24-hour Orthopedics, Neuro sciences & Accident Trauma Centre.
TYPES OF HEADACHE
Tension-type headache is the most widespread of headache disorders. Onset is often in the teenage years and prevalence peaks in the fourth decade and then declines. Tension-type headache is more common in women, develops gradually. It often involves the entire head as well as the neck and shoulders. It is probably caused by increased muscle tension, although not agreed by all specialists. Most people get tension headaches occasionally and these can usually be treated simply. Some people get them often, but there are usually some useful interventions to help decrease the number of sick days. A migraine headache is throbbing, moderate to severe pain, usually on one side of the head, that is worsened by physical activity, light, sounds, or smells and may be associated with nausea and vomiting. There are mainly two types of migraine, classic and common. The basic difference between the two types of migraine is the appearance of an ‘aura’ seen in classic type. The aura is the occurrence of neurological symptoms 10-30 minutes before the attack. You may see flashing lights, zigzag lines or may temporarily lose vision. Other symptoms of classic migraine include speech difficulty, confusion, arm or leg weakness and tingling of face or hands. The pain of a classic migraine headache is described as an intense throbbing or pounding felt in the forehead/temple, ear/jaw or around the eyes. Classic migraine starts on one side of the head but may eventually spread to the other side lasting for one or two days. The common migraine is more ‘common’ and not preceded by an aura. Some people do experience a variety of vague symptoms before common migraines mental fuzziness, mood changes, fatigue, and unusual retention of fluid. During the headache phase of a common migraine, you may have abdominal pain and diarrhea, increased urination, nausea and vomiting. Both classic and common migraines can strike as often as several times a week or rarely as once every few years. Cluster headache is an extraordinarily painful, rare chronic disease more common in men. Cluster headaches usually develop between the ages of 20 and 40. The term ‘cluster’ is used as the attacks usually occur in groups or clusters, typically for several weeks once or twice a year at the same time of year. People with cluster headaches often describe the pain as similar to an ice pick. Sinus headaches are those frontal headaches that some people experience with sinus infection and with changes in the weather. Allergies can also provoke them.
HEADACHE TRIGGERS
Although the tendency to have frequent headaches is probably inherited, the way you live your everyday life could influence how often those headaches occur. If headaches are a serious problem for you, it makes sense to pay extra attention to factors that could trigger or aggravate headaches. Potential headache precipitating factors (triggers) are many and varied. Different types of headaches have different triggers. Triggers are not the same for everyone, and not necessarily the same for different attacks in the same person. Identifying triggers may be complicated by the fact that it often takes a combination of triggers to set off a headache. For example, a stressful day followed by a few glasses of red wine that evening and oversleeping the next morning might trigger a migraine whereas red wine at lunch may have no effect. It is important to understand your trigger factors and avoid them as far as possible.
- Stress and time pressure, major hassles, major losses, anger and conflict.
- Smells and fumes, tobacco smoke, light glare or dazzle, weather changes.
- Monthly periods, birth control pills, estrogen therapy.
- Sleep disturbances.
- .Hunger, fasting, specific foods or beverages. (See table 1.)
- Excessive physical strain.
- Cheese, beer, wine, hard liquor, coffee, tea, cola, chocolates, pizzas, seasoned Salt, canned soups, snack chips, saccharin, ice cream, milk, yogurt, pickles, oranges, grapes, lemons, onions, bananas, peanuts, sandwich meats, hotdogs, fresh breads etc.
MANAGEMENT OF HEADACHE
Headache management is indeed a great challenge. A number of treatment options, preparations and methods of administration may have to be tried to discover what works best for each headache sufferer. The role of the doctor is vital in this process. Once your headache is correctly diagnosed, your headache management plan can be developed. The plan should be evaluated and updated regularly. While there is still no absolute cure for headache, there are a number of treatment options, both medications and other forms including complementary therapies. Always consult your medical practitioner. Some medications are given once the headache has begun (acute treatment) and others are taken daily to reduce the frequency of attacks (prophylactic treatment). Acute episodes are treated by various analgesics. Prophylactic medication is taken daily, regardless or whether a headache is present, to reduce the incidence of severe or frequent headaches. Your doctor will be able to help you find out what type of medication is best suited and safest for your needs.
COMPLIMENTARY THERAPY
This offers a natural solution to pain relief and headache management. There are a number of options available. Most are concentrated on releasing tension in the body, thus easing pressure in the head. Not all these options will work or be available to everyone. A healthy lifestyle may help reduce or eliminate headaches or will at least improve your overall health. Eating healthily and regularly, drinking less caffeine and alcohol and plenty of water, exercising regularly, avoiding fatigue and having plenty of rest, having sufficient regular sleep, good posture and ensuring that work and living areas are well ventilated and well lit. Stress management involves learning to be able to control stress and relax. Everyone has periods of stress. Stress has benefits in that it can result in us pushing ourselves and getting things done. This can precipitate a headache. Simply taking some deep breaths and maybe tensing then relaxing your muscles can relieve occasional mild stress. Regular stress may require learning to say ‘no’, not taking too much on. Becoming fit, eating regularly, and proper sleep can help combat stress. Learn better organizing skills, not setting standards that are too high and deal with problems as they arise, can all help. As can, adopting stress management techniques such as meditation, biofeedback, relaxation therapy and yoga.
NEURONAVIGATION SURGERY: NAVIGATING INSIDE YOUR BRAIN!
The same technology that used to bring Godzilla to life in the movies also is being used to help surgeons in the operating room perform tasks such as placing new hip joints or reaching difficult brain tumors. Today, many hi-tech hospitals around the world utilize image guided surgery to plan and help surgeons navigate through the body. These advances have made great strides in the patient care and outcome in neurosurgery. HOSMAT Institute of Neurosciences recently has procured an advanced Brain Lab Neuronavigation system which is the first installation in the country as of now. This system consists of sophisticated computer systems which use infrared rays to guide the surgeon during the surgery. A 61-year-old lady developed sudden onset of headache and weakness of left side of her body since 8 days. She was evaluated by a neurologist and subsequently referred to us for management. MRI scan of her brain revealed a brain tumor known as glioma in her right brain. The tumor was located on a highly sensitive area called ‘Motor strip’ which is responsible for the movements of the limbs. The brain tumor found in her is a type of ‘glioma’ which is very aggressive tumor to tackle. The main concern for neurosurgeon in this case was the proximity of the tumor to the ‘Motor strip’. In conventional neurosurgical procedure, the tumor is removed based on surgeon’s visualization. In some types of tumors, surgeons may not completely visualize the tumor due to various reasons. If normal brain is unduly handled, it can cause significant problems like paralysis, loss of speech, blindness etc. By using Brain Lab neuronavigator, our team of doctors removed the tumor completely. The patient is recuperating in the ward. She is made to walk on the very next day and her weakness is corrected totally.
THE HISTORY OF BRAIN SURGERY
Brain surgery is perhaps the oldest of all practiced medical arts. There is evidence of brain surgery as early as 3000 BC in Africa. Back in those times, surgeons did not know about the function of the brain as studying dead bodies was considered a sin. But, as the facts about brain and its functions was known, surgeons were more careful and precise in dealing with it. When treating brain tumors, tumor resection is the initial treatment. Until recently, open neurosurgery meant a fairly high risk for patients in terms of damaging important structures of the brain. Today, computer-based neuronavigation or image-guided surgery assists the surgeon during all phases of the operation. This allows the surgeon to keep the operation minimally invasive and to avoid critical structures of the brain. Thus, the risks of paralysis or other impairments after surgery are minimized and recovery time is considerably reduced.
WHAT IS IMAGE-GUIDED SURGERY?
Image-guided surgery has been employed in neurosurgery since the mid-1990s. This new technique relies on a powerful computer system, which assists the surgeon in precisely localizing a lesion, in planning each step of the procedure via a 3D model on the computer screen, and in calculating the ideal access to the tumor before the operation. The tumor and its surroundings can be viewed from different angles and in relation to landmark structures, such as the optic nerve or the brain stem. During the operating procedure, the movement of the instruments in use inside the brain can be tracked on the monitor with a precision of 1-2 millimeters, through which damage to healthy tissue and to critical areas can be avoided as much as possible. The tumor’s location and its position relative to the sensitive structures in the brain will be pinpointed so that sensitive structures can be avoided and the incision can be kept as small as possible. This is particularly useful in reaching a tumor located deep within brain areas traditionally considered to be difficult to reach. During the procedure, the computer tracks instrument movement with an extremely high precision, providing the surgeon with total control inside the brain at all times using “real-time” imaging. The surgeon can also check if the tumor has been removed as planned. This improves the outlook for the patient.
WHAT TYPE OF SURGERY CAN BE PERFORMED IMAGE-GUIDED?
A stereotactic biopsy is performed in order to obtain an exact diagnosis of the tumor and to differentiate the tumor from healthy tissue or infective tissue. A small tissue sample is obtained from a defined region of the brain by using a long and very thin needle, which is passed through a skin puncture and tiny opening in the skull to the location of the tumor. The tissue sample is then examined by a pathologist and the nature of the lesion is determined. If the lesion proves to be a tumor, the type of tumor will be determined. The image-guided surgery system assures that the tissue sample is taken from the area of interest and not accidentally from the neighboring region. Most patients are discharged from the hospital the very next day.
CRANIOTOMY
The most commonly performed surgery for the removal of a brain tumor is called a craniotomy. The objective of the surgery is to excise as much of the tumor as possible. Even if only a portion of the tumor can be removed, this can still lead to an improvement of symptoms. For the surgery, a portion of the scalp is usually shaved, and an incision is made through the skin. A piece of bone is removed to expose the area of brain over the tumor, then the tumor is removed. After the tumor has been removed, the bone is generally replaced and the incision closed. In a conventional craniotomy, surgeons guide themselves by what they can visualize, their knowledge of anatomy and their interpretation of the pre-operative scans. This is purely a ‘hand to eye’ technique. With the use of this technology, the tumor as well as different brain structures can be well identified and viewed on the computer screen. The surgeon can navigate precisely to the tumor while avoiding sensitive structures. The depth of the tumor can be mapped, as well as critical structures that might lie on the other side of the resection plane. Such navigation increases the precision of the procedure, and can increase the speed at which surgery can be performed.
SHUNT
Occasionally, patients with brain tumors develop increased intracranial pressure due to accumulation of excess fluid in the ventricles (brain chambers). To relieve the pressure, a shunt procedure to drain excess or blocked fluid might be necessary. A small hole is drilled in the skull through which a catheter is inserted into the brain chamber. The other end of the tubing is threaded to the abdomen from where the fluid is absorbed.
IMPLANTS
In many cases, patients with brain tumors are treated by the insertion of radioactive material (brachytherapy) or genetic material into the cavity left by the tumor’s removal. Neuronavigation is able to ensure the accurate placement of an implant into the defined area.
FUNCTIONAL NEUROSURGERY
Mapping tools can improve the safety and effectiveness of surgery by locating the exact areas of the brain responsible for speech, comprehension, sensation or movement. Specific areas of the brain are stimulated by a tiny electrical current, through which their functionality can be determined. This allows these areas to be avoided during surgery.
WHAT ARE THE ADVANTAGES OF NEURO NAVIGATION?
- Proper definition of the ‘target area’ by detailed 3D reconstruction.
- Precise placement of the craniotomy flap.
- Accurate delineation of tumor and vital brain structures.
- Identification of eloquent areas of brain and their preservation.
- Minimal brain handling: minimally invasive neurosurgery.
- Reduces morbidity overall.
SUMMARY
- Image guided neurosurgery is the result of constant research to improvise the surgical technique and results
- Provides excellent guidance to surgeons especially while operating on critical brain areas.
- Provides excellent guidance to surgeons especially while operating on critical brain areas.
IS IT MERELY A PAIN IN YOUR NECK?
Our head and neck region is vulnerable to many different stresses. Bad posture can cause misalignment of your neck, head, and spine. Car accidents can cause whiplash. Age and wear and tear can cause arthritis. Even activities such as gum chewing and reading in bed can cause pain. How do we avoid these potential problems? And if we cannot avoid them, how can we recognize them and cope up with them ? Have you ever been tried to grab something just out of reach on an upper shelf of your wardrobe, and felt an immediate catch in your neck? Or did you ever wake-up in the morning on your sofa, and have a painful, stiff neck that left you barely able to move your head a whole day? The chance of you answering ‘ yes’ is nine out of ten. You are not alone! Neck pain is one of the common visits to clinics now a day. Most neck pain is caused by muscle strain or sprain, and although some people have this pain for a long time, it is usually not serious. One of the most flexible regions of the spine is the neck (cervical) region, which consists of vertebrae, seven shock-absorbing discs, muscles, and vertebral ligaments to hold them in place. The uppermost cervical disc connects the top of the spinal column to the base of the skull. The spinal cord, which sends nerve impulses to every part of the body, runs through a canal in the cervical vertebrae and continues all the way down the spine. The cervical nerves spread down into the arms; because of this, arm pain is sometimes traceable to a problem in the neck. While most people do not have serious medical problems, neck pain could be the sign of an underlying condition that requires medical attention. Neck pain may be caused by disc degeneration, narrowing of the spinal canal, spondylosis, arthritis, and, in rare cases, cancer or meningitis. For serious neck problems often a specialist such as a neurosurgeon should be consulted for an accurate diagnosis and proper treatment. The neck is supported at the back by a staircase of seven bones called cervical spine. They are separated by what is known as a disc. These bones, discs and joints are prone for a variety of disorders that can result in a ‘bad neck’. Advancing age, injury, bad posture, or diseases such as arthritis can lead to degeneration of the bones or joints of the cervical spine, causing disc herniation or bone spurs to form. Sudden severe injury to the neck may also contribute to disc herniation, whiplash, vertebral injury, and, in extreme cases, permanent paralysis because of spinal cord injury. Herniated discs or bone spurs may narrow the canal through which the spinal cord runs or narrow the small openings through which spinal nerve roots exit. Pressure on a nerve root from a herniated disc or bone spur may cause pain in the arm and neck, numbness or weakness in the arm, tingling in the fingers or hand and difficulty in walking. Cervical canal stenosis occurs when the spinal canal narrows and compresses the spinal cord and is most frequently caused by aging. The discs in the spine that separate and cushion vertebrae may dry out. As a result, the space between the vertebral bodies shrinks, and the discs lose their ability to act as shock absorbers. At the same time, the bones and ligaments that make up the spine become less pliable and thicken. These changes result in a narrowing of the spinal canal. In addition, the degenerative changes associated with cervical stenosis can affect the vertebrae by contributing to the growth of bone spurs that compress the nerve roots. All these result in neck pain, numbness and weakness in both hands, unsteady gait when walking, and muscle spasms in the legs. Mild stenosis can be treated conservatively for some time long as the symptoms are restricted to neck pain. Severe stenosis requires referral to a specialist neurosurgeon. In addition to performing a thorough examination, a neurosurgeon may order diagnostic tests to help determine the cause and severity of your neck pain. These tests include x-rays, CAT scans, Magnetic Resonance Imaging (MRI), Electromyograms and Nerve Conduction Studies (EMG/NCS). A spinal tap for a cerebrospinal fluid analysis may be needed if meningitis (infection of the coverings of the brain) is suspected.
WHEN TO CONSULT YOUR DOCTOR FOR NECK PAIN?
- If it occurs after a blow to the head or neck.
- If neck pain along with fever or headache.
- If stiff neck prevents you from touching your chin to your chest.
- If pain shoots down one of your arms.
- It there is tingling, numbness or weakness in your arms or hands.
- If your pain does not respond to over-the-counter pain medication in a few days.
- If pain does not improve after a week to ten days.
Non-surgical (conservative) treatment is the first approach in patients with common neck pain not involving trauma. For example, many patients with cervical disc herniation’s improve with conservative treatment and time and do not require surgery. Conservative treatment includes pain medication, collar, traction, bed rest, and physical therapy. Your doctor may prescribe medications to reduce the pain or inflammation. Sometimes an injection of corticosteroids may be used to temporarily relieve pain. Your neurosurgeon may advise surgery if you experience progressive neurological symptoms involving your arms and legs. Type of surgery varies depending on your disease, symptoms and MRI findings.
BUT IS THERE ANY WAY TO PREVENT NECK PAIN?
One of the most common causes of neck pain is poor posture. It is easy to get into bad posture habits without even realizing it -even an activity as ‘innocent’ as reading in bed can sometimes cause neck pain. The goal of ‘good posture’ is to keep your head centered over your spine, so gravity works with your neck instead of against it. Try these simple steps to a healthy neck!
TAKE FREQUENT BREAKS
if you drive long distances or work long hours at your computer. Keep your head back, over your spine, to reduce neck strain. Try to avoid gritting your teeth.
ADJUST YOUR DESK
Chair and computer so the monitor is at eye level. Knees should be slightly lower than hips. Use your chair’s armrests.
AVOID TUCKING THE PHONE
Between your ear and shoulder when you talk. If you use the phone a lot, get a headset.
STRETCH FREQUENTLY
If you work at a desk. Shrug your shoulders up and down. Pull your shoulder blades together and then relax. Pull your shoulders down while leaning your head to each side to stretch your neck muscles.
BALANCE YOUR BASE
Stretching the front chest wall muscles and strengthening the muscles around the shoulder blade and back of the shoulder can promote a balanced base of support for the neck.
NO TUMMY SLEEPING PLEASE
That position puts stress on your neck. Choose a pillow that supports the natural curve of your neck. Reading in bed can cause neck strain, especially if you’re propped up on several pillows.
PILLOW TALK
Does your pillow cause you to sleep with your neck at an angle, either too high or too low? If so, you may have to invest in a new pillow soon!



